COVID-19 and the NHS: Disruptive Transformation?
Authored by Jo Cubbon, Alamac Chair and seasoned NHS Leader
COVID-19 and the NHS: Disruptive Transformation?
After weeks of the spread of the COVID-19 pandemic and widespread lockdown, we must begin to take stock of how the crisis has disrupted the NHS whilst also creating opportunities for widespread transformation. Chancellor Rishi Sunak said, ‘Innovation and entrepreneurship have powered growth in our country for centuries and it is what will drive our growth as we recover from this crisis.’
The focus is shifting from responding to the crisis to recovery. This quite rightly starts with areas where COVID-19 disruption must not, and cannot, be continued because it threatens to de-stabilise the fabric of the NHS and the care of patients. However, the NHS must also start to understand where there has been positive ‘disruptive transformation’ which must become the ‘new normal’. Over the past few weeks, the service has seen dramatic and extensive changes to so many delivery pathways;
Urgent Care
A&E attendances have dropped in England to the lowest level since records began. And they dropped quite literally off a cliff with the national position shown below:
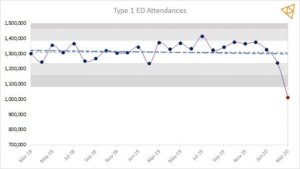
We know that there is cause for concern in this – West Midlands Ambulance Service reported 300 people refusing to be conveyed to hospital after being assessed by a paramedic and there is a suggestion that this may be the tip of the iceberg in terms of the health problems which will emerge post COVID19.
We also know that changes to the patterns of behaviour as a result of lockdown measure have changed demand for emergency services. Some injuries have legitimately reduced (for example fewer car journeys resulting in fewer RTAs) and people have legitimately sought support in more appropriate settings – by phone (111), in primary care, pharmacies and in other community services. Indeed, the level of transformational disruption for Urgent Care has the potential to far exceed any of national initiatives such as the UEC Vanguards and has impacted significantly on hospital demand, flow and capacity.
Hospital Discharge
Whilst DTOC figures aren’t being recorded during this period we know from looking at data at an organisational level that discharge delays have more than halved and with this has come solutions for those patients that would historically have stayed in hospital for more than 21 days.
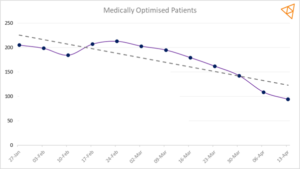
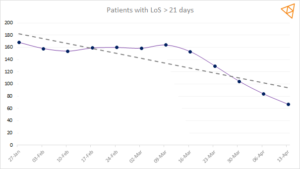
(typical medium sized Acute Trust)
Hospital Discharge Service Requirements were issued by NHS England on 19th March, however systems had been working hard and were already on a trajectory of reducing delayed patients; arguably this guidance provided continued support by removing the need for some assessments in a hospital environment. There may be lessons to be learned here on the impact on other providers including around the appropriateness of discharge into Care Homes and some detail to understand the impact of spend on residential care beds. But there has been undoubtedly some disruptive transformation – decisions are made faster through a central point in the hospital, ‘home first’ type services have been created by community teams and, most importantly, people are only in hospital for the time they really need to be.
Primary Care
At the end of March, Primary Care practices were urged to move to a Triage First model of care and provide online services where they can, to support the national Covid19 response. Online consultations became the ‘new normal’ overnight, with a surge in the uptake of digital GP services to support the response, with many tech companies offering their services to the NHS for free.
The NHS App, which was made available to the public in January 2019 and gives people access to NHS services, such as booking appointments and viewing their medical records had been downloaded 915,500 times in the 25 months to 24th February 2020. In 2 months from 24 February, when NHS Digital launched its Covid-19 response, the NHS App has been downloaded nearly 434,000 times. More than 100,000 requests for repeat prescriptions have been made since 24 February, compared to 236,000 in the whole year prior to the pandemic.
Yet along with disruptive transformation comes a threat. In a comment to HSJ, Professor Marshall Chair of the Royal College of General Practitioners warned that, while remote consultations are “necessary” to prevent the spread of coronavirus, some mental health patients “may find it difficult” to adapt to digital appointments. This is one group of patients who are likely to be suffering through lockdown without access to services – and there could be more.
Outpatients and Elective Care
In the second week in April 2020, NHS England asked Trusts to suspend all non-urgent elective operations for at least three months to ensure the NHS had the staffing, bed and ITU capacity to cope with a surge in critically ill patients. The elective waiting list already stood at 4.4 million patients before the outbreak, the highest figure since the referral to treatment pathway began in 2007.
Trusts saw daily elective admissions drop to near zero in the space of 6 weeks:
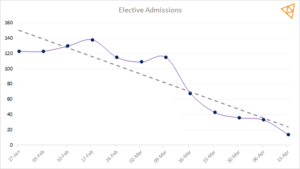
(typical medium sized Acute Trust)
When asked in mid -March about the potential impact of COVID19 on NHS elective waiting times, Rob Findlay of Gooroo noted that: ‘a three-month covid-19 shutdown might add about 5 months’ worth to that existing waiting list growth, or less than a week on top of the existing 25-week RTT waiting times’ and suggested that ‘the covid-19 shutdown might particularly affect those patients who are already waiting the longest, and who are already most at risk of clinical harm because of their wait.’
Many thousands of face to face outpatient appointments have been cancelled, but all is not lost. Many have been replaced with telephone and online consultations and alternative care pathways have been developed. Many interesting and creative patient stories and experiences are emerging; A 90-year-old lady from Cirencester waiting for her hearing aid had her hospital appointment cancelled. Had she attended previously this would have involved transport to and from the hospital, packing continence pads in case she could not find a loo and worries about navigating her way to the audiology department. Instead she had a telephone consultation explaining all about how she used her new hearing aid which arrived the next day by post – and she was delighted!
One large teaching Trust cancelled over 140,000 outpatient appointments over the three-month period. One big question the teams are now asking is – were they all needed? Understanding this has big impacts on resource planning for the future; staff, facilities, infrastructure and equipment required.
Community Services
‘Communities’ has taken on a whole new meaning in so many areas. Neighbours and are helping those who are vulnerable and isolated, supporting many of their care and social needs, resulting in lower demand for the more ‘‘traditional’ care services. In turn many of the community care givers are experiencing a greater and improved sense of purpose and well-being. A London based daughter recently thanked a village community for supporting her 98 year- old isolating mother for caring for all her needs; meals, cleaning, prescription collection and personal support over the past 4 weeks. During that period, she had had no contact with her GP and has declined to use her domiciliary care provider. Transformational disruption has delivered the concepts of ‘place’ of ‘strengths-based practice’ and of ‘neighbourhoods’ quite literally overnight.
Counter to this, lockdown measures have created a level of isolation which poses a threat to the most vulnerable in society and we await with some apprehension a greater understanding of the impact on those with disabilities, those experiencing domestic violence and vulnerable children and adults in our communities.
Conclusions
So much has changed over the past weeks and the NHS must now prepare to understand the impact using robust evidence and analysis. We must restore what we know works well, retain the good practice that has proved effective during our period of disruptive transformation, and recover the areas where the disruption which is not best for patients.
We are working with NHS Trusts, CCGs and ICSs on the first stage of their disruptive transformation journey, gaining insight through data, seeking to answer a whole set of questions such as:
- Who are the cohorts of people we are likely to be missing from A&E and who are the people we need to make sure can continue to use alternative services in the community? What should an ED of the future look like and how should it operate?
- How do we get back on track with elective care? How can we optimise our current capacity to deliver this?
- What impact can the use of telephone and digital consultations have on outpatients and in primary care in the future?
We will share that insight as it emerges. If you are interested in joining our programme of work to explore these issues, please contact the team:
Paul Brandwood
T 07932 594 968
E Paul.Brandwood@vitalhub.com